Abstract
Several prognostic models have been developed to identify patients at high risk of death, treatment resistance, or poor survival after conventional intensive chemotherapy in older adults with acute myeloid leukemia (AML). There are growing evidence that geriatric assessment can detect unrecognized vulnerabilities in patients with hematological malignancies to help predict treatment tolerance and survival. We prospectively demonstrated the prognostic value of physical function for survival outcomes in intensively treated older adults with AML (Min et al. Blood 2022). However, there are limited evidence for prognostic value of physical function in older adults with AML who were treated with low-intensity therapy, such as hypomethylating agents (HMA) with or without venetoclax (VEN). Thus, we evaluated the prognostic role of physical function scores in older adults with AML treated with low-intensity treatment in a prospective observation cohort (CRIS number; KCT0002261).
We have measured physical function by the Short Physical Performance Battery (SPPB) since 2018 in older adults with AML treated with low-intensity treatment. Between 2018 Jan and 2022 May, 71 newly diagnosed AML patients who were aged ≥ 65 years and received low-intensity treatment were examined with SPPB at a median of 3 days prior to the initiation of treatment. The prognostic role of SPPB score on overall survival (OS) was analyzed by the Kaplan-Meier estimates and the log-rank test, and a multivariable Cox hazard model.
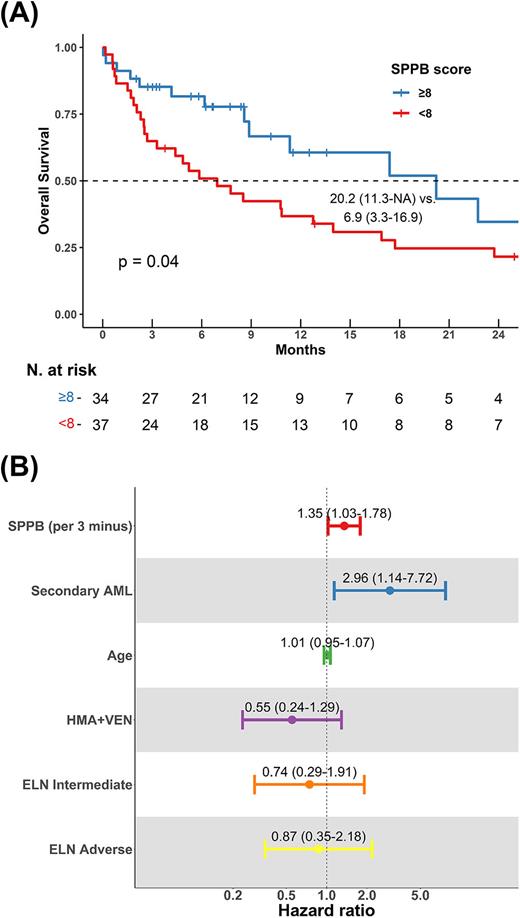
The median age of 71 patients was 75 years (interquartile range: 70-78). Males were 59.2%, and patients with an Eastern Cooperative Oncology Group (ECOG) score of 2 or higher was 19.7%. Secondary AML patients were 12.7%. Genetic risk stratification by European Leukemia Net (ELN) 2017 classified 23.9%, 36.6%, and 39.4% as favorable, intermediate, and adverse risk, respectively. Patients were treated with HMA alone (azacitidine or decitabine; 59.2%) or HMA and VEN combination (40.8%). Seventy percent of patients were classified as unfavorable group by Wheatley index, which is a validated prognostic model for low-intensity treatment. There were no differences between HMA alone and HMA and VEN combination in terms of Wheatley index. The median SPPB score of patients was 8 (range, 6-11). The SPPB score had a significant association with OS. In univariable analysis, the hazard ratio (HR) for a 3-point decrease in SPPB was 1.11 (95% confidence interval [CI], 1.02-1.20]. The cut-off of SPPB at which the difference in OS was most pronounced was 8. Patients with an SPPB score of 8 or higher had a median OS of 20.2 months (95% CI: 11.3-Not achieved), whereas that of patients with an SPPB less than 8 was 6.9 months (95% CI: 3.3-16.9, p=0.04, Figure A). In a multivariable Cox model of SPPB with other genetic, etiologic variables, the impact of SPPB on OS was still significant (HR for 3-point decrease in SPPB: 1.35 [95% CI: 1.03-1.78], Figure B).
Our data show that physical function measured by SPPB is a significant prognostic factor for survival in older adults with AML treated with low-intensity treatment, contrasting limited value of 2017 ELN. This suggests that specified prognostic models including diverse geriatric assessment domains should be studied in these elderly population treated with low-intensity treatment.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal